Anesthesiology Assistants (AAs)
ARE NOT
The Same as CRNAs
CRNAs ARE PROVEN PROVIDERS WITH A >150 YEAR HISTORY OF QUALITY CARE
Just THE FACTS about
Certified Anesthesiologist Assistants (CAAs)
- Used as an Anti-Competitive Tool: Though the first AAs graduated in 1970, the ASA did not take any interest in supporting their profession until 2001, the same year “opt out” was created. For the ASA, AAs are just a retaliatory and controllable response to CRNAs making progress toward working to full scope of practice. They became another tool in the ASAs anti-competitive and trade protectionist fight to limit CRNAs from expanding access to high quality care in a cost- effective manner. (https://tinyurl.com/yjq3sg68)
- Trained to Assist, not Independent: AA programs range in length from 24-29 months. They graduate with a masters degree and their training is focused on ‘assisting’ the physician anesthesiologist not on expert level independent practice, as it clearly states “assistant” right in their title.
- No Previous Healthcare Experience or Degree: There is NO requirement for any clinical experience prior to entry into AA school. This is divergent from the other three expert anesthesiology professions Dentists, Physicians and CRNAs who all have previous healthcare training before undertaking specialty training in anesthesiology. While these three professions all have a depth of knowledge related to disease process/treatment, testing interpretation, anatomy/physiology, critical thinking, experience with critically ill patients etc., AAs are discovering where the stickers go for an EKG for the first time. This effectively is lowering the existing standard. (https://tinyurl.com/yj4egwc9) (https://tinyurl.com/yk5gn6oc)
- AAs are Deceptive About Their Clinical Hours: AAs talk about 2000 hours of clinical time but unlike CRNAs they count every lab, certification course and minute in a hospital even when not performing anesthesia. When counted the same way CRNAs have over 8636 hours of relevant clinical time with patients and anesthesia. (https://tinyurl.com/yjw7crho)
- They Cannot Actually Impact the Shortage: There are under 4000 AAs after existing for over 50 years and they only graduate about 300 AAs per year. In contrast there are over 60000 CRNAs who can practice anesthesia independently graduating over 3000 per year. Just from a numbers perspective it is clear AAs are not the answer to any shortage concerns. (https://tinyurl.com/yjamq56z)
- Work as Assistants & Can’t Alleviate Shortages where they Matter: AAs can ONLY practice where physician anesthesiologists work and under their direct supervision in a 1:4 (or less) ratio. The vast majority (over 90%) of physician anesthesiologists work in urban areas. This means AAs cannot alleviate shortages in underserved and rural areas where the need is by far the greatest. CRNAs have no such restrictions and can work autonomously in teams with physicians and independently anywhere in the nation in any practice and without costly ratios.
- Can Only Work in the MOST Expensive Model: AAs can only work in the MOST expensive model of care which is neither efficient nor cost effective. If all 55,000 physician anesthesiologist actually performed anesthesia in an operating room as opposed to watching others do so there would be no shortage. This does not serve anyone except those who seek to control the market.
- AA ≠ PA: Anesthesiologist Assistants are NOT Physician Associates (PAs). Whereas PAs are fully trained and functioning healthcare providers, AAs are trained to assist someone else. They are not the same. (https://tinyurl.com/yjcfr8fa) (https://tinyurl.com/yfnkqoux)
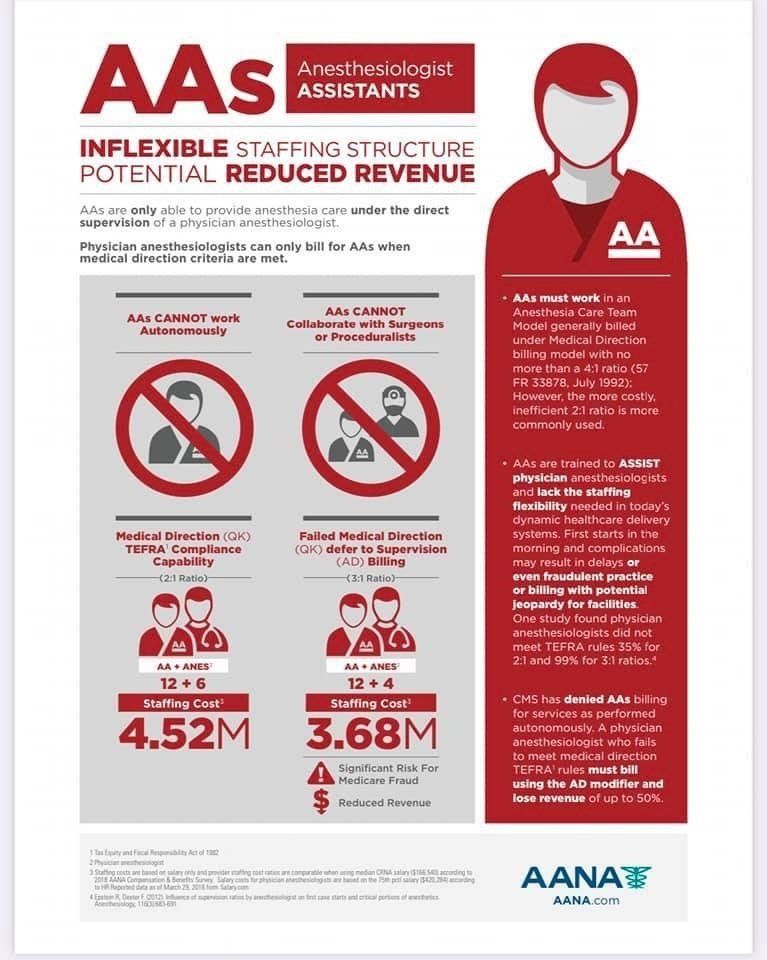
- They Create Fraud Risk for Facilities: The use of AAs is high risk for medicare fraud even in a 1:4 ratio. In the ASA Epstein study (https://tinyurl.com/yemno76a) it showed that medicare fraud was committed 35% of the time in a 1:2 ratio, 99% in 1:3 and 100% in 1:4 ratio. To avoid fraud = delay cases = less cases per day = decreased access for patients with same costs (OR still there now less efficient). Since CRNAs are independent experts in anesthesiology and not required to work under supervision this is a non-issue. (https://tinyurl.com/yggh2e54)
- Only Physician Anesthesiologists can train Assistant AAs: CRNAs cannot train AA students yet CRNAs perform more than 70% of all anesthetics nationally. Most physician anesthesiologist are not in the operating room. Who will train them? (https://tinyurl.com/ygg9pnd4)
- AAs Are Assistants - They Cannot Train CRNA Residents: When AAs enter a practice fewer CRNAs can be trained. Independently trained and practicing CRNAs are the answer to cost containment and access to care, why limit training the solution in favor of AAs who can only work in the most expensive model in big cities? (https://tinyurl.com/yj75tho5)
A special thanks to Dr. Michael McKinnon, DNP, FNP, CRNA for his contributions to this page.
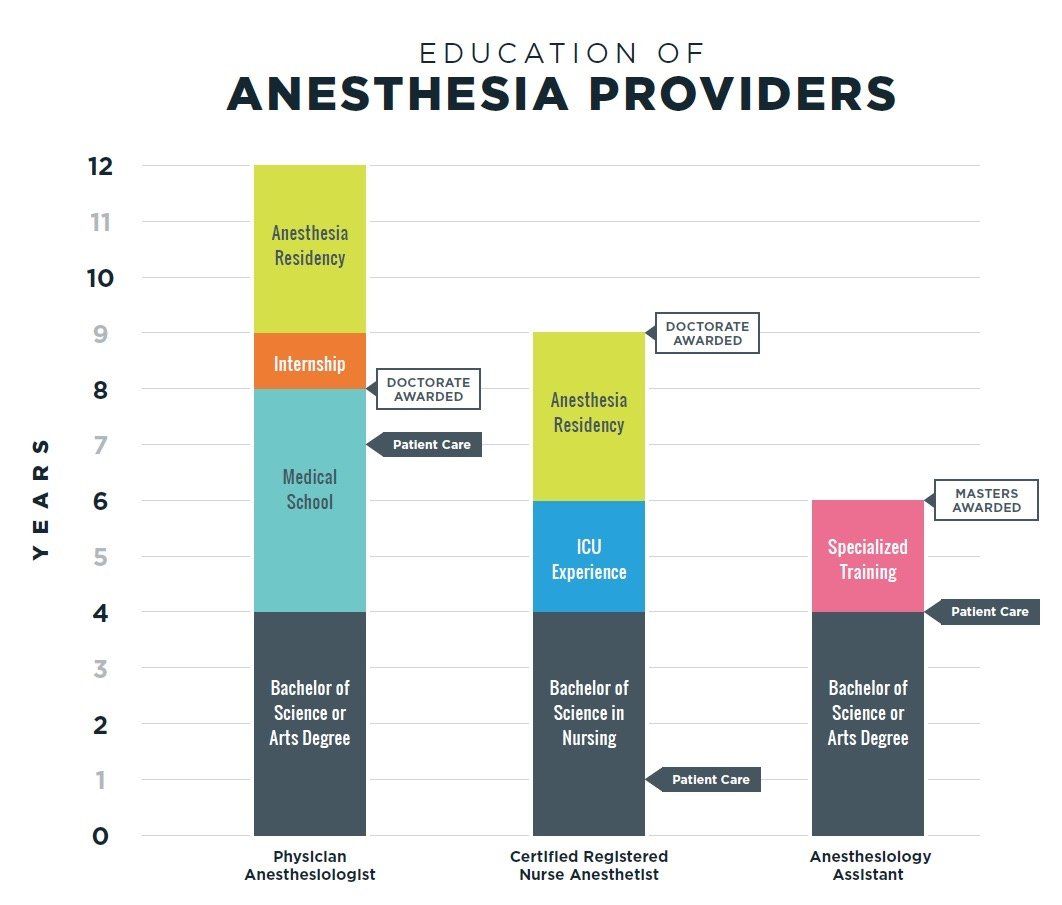
Note: Only CRNAs begin hands-on patient care within their first year of training. This results in CRNAs having a minimum of 8 years of actual patient care before becoming a board certified provider - more than any other anesthesia provider.
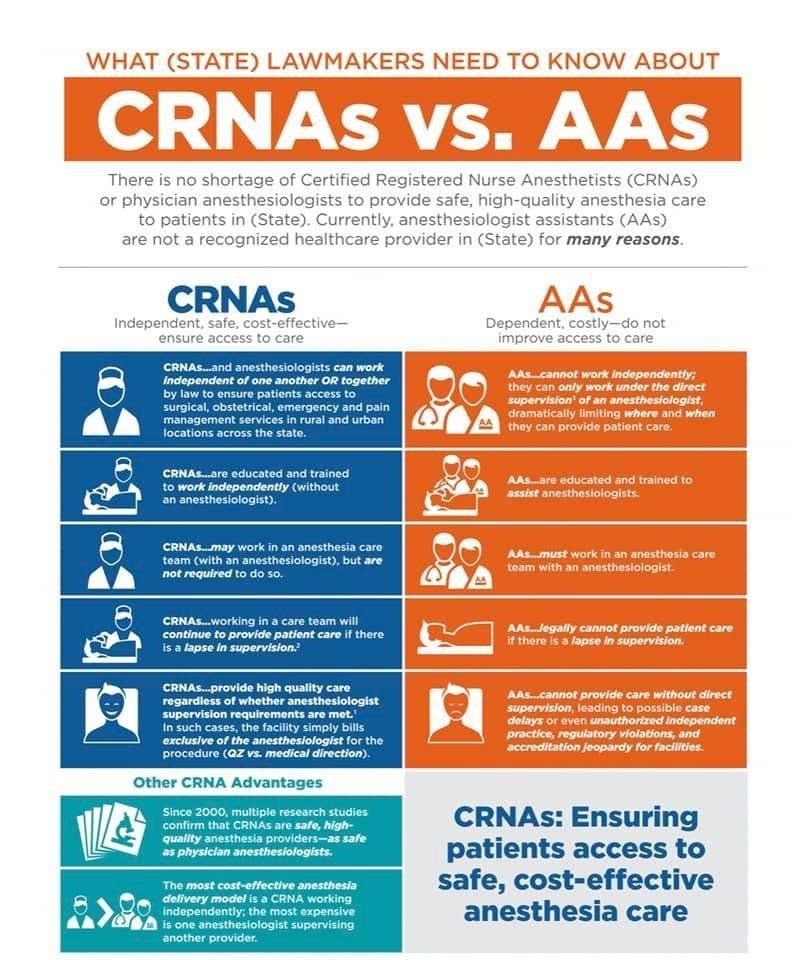
Note: AAs DO NOT address anesthesia provider shortages. Because they are a dependent provider they must work with a physician anesthesiologists which creates a model where TWO providers are paid instead of ONE. Eliminating the anesthesia care team model (ACT) increases provider access by utilizing the complete skill sets of both physician and nurse anesthesiologists as independent providers.
Note: Anesthesiologist Assistants INCREASE cost of anesthesia services and DECREASE access to care. An AA's education and training is designed to produce a dependent provider that fails to provide the expertise necessary for the delivery of superior patient care independently.