WHAT OPT-OUT DOESN'T MEAN
1) Opt-Out has NOTHING to do with CRNA scope of practice - it doesn't expand or contract what a CRNA can do. CRNA Scope of Practice is defined by the AANA and to a lesser degree by state law or even facility bylaws.
- CRNA scope of practice is determine by local practices and the facility by-laws. NOT Medicare Conditions of Participations (CoP).
- Opt-Out specifically addresses the ability for a hospital and facility to bill for the anesthesia services provided by a CRNA - nothing else.
- Opt-Out STRICTLY DEALS WITH FACILITY REIMBURSEMENT
2) Opt-Out does not eliminate the need nor the practice of CRNAs collaborating with various specialized physician and/or APRNs - as the goal is always to ensure patient safety and/or optimization a particular patient co-morbidity. This is no different than a physician would do. Specialty - CRNA relationships are unaffected, and in reality, are probably enhanced in many ways by CRNA independent practice.
3) Opt-Out does not create an increased safety risk for patients who receive their anesthetic care from an unsupervised CRNA - to date, 22 states and Guam have opted out.
- Although the Medicare/Medicare 'Conditions of Participation' (CoP) require a CRNA to be supervised by a physician, dentist, or podiatrist, they are not required to be trained in anesthesia nor actually be a physician anesthesiologist.
- To date, 22 states and Guam have opted-out of the CoP supervision requirement. Since the first state, several empirical studies, including and extensive analysis by the Cochrane Foundation, have demonstrated that the care delivered by an unsupervised CRNA is just as safe, if not more safe, than care delivered by an MDA only or MDA working with a CRNA model.
WHAT DOES OPT-OUT MEAN?
- Opt-out specifically addresses "Part A" of the Center of Medicare & Medicare (CMS) requirements, aka the Conditions for Participation (CoP), for hospitals and facilities to be reimbursed Medicare and Medicaid dollars for anesthesia services that are provided by a CRNA. It does NOT have any bearing on Part B which addresses reimbursement for actual services rendered by a CRNA provider.
- The federal requirement for CoP has been that CRNAs must be supervised by a physician, any physician not necessarily a physician anesthesiologist, in order for the hospital or facility to be reimbursed by CMS. The November 13, 2001 rule allows states to "opt-out" or be "exempted" (the terms are used synonymously in the November 13 rule) from the federal supervision requirement.
- Thus, in opt-out states, hospitals and facilities that provide healthcare and anesthesia services provided by a CRNA are qualified to collect funds from CMS for those services without meeting the physician supervision requirements or guidelines. In short, this allows for many facilities across the country, especially in rural areas, to collect much needed revenues for those services without the unnecessary oversight. Since 2001, 21 states plus Guam have opted - out of this burdensome supervision requirement without sacrificing the quality of care provided.
- For a state to "opt-out" of the federal supervision requirement, the state's governor must send a letter of attestation to CMS. The letter must attest that:
- The state's governor has consulted with the state's boards of medicine and nursing about issues related to access to and the quality of anesthesia services in the state; and
- That it is in the best interests of the state's citizens to opt-out of the current federal physician supervision requirement; and
- That the opt-out is consistent with state law.
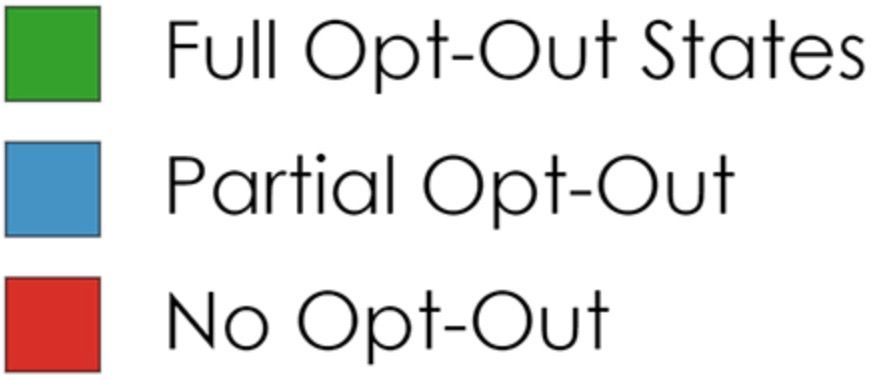
HOW MANY OPT-OUT STATES ARE THERE? 21 states and Guam have opted out. States that have opted out are Arizona, Arkansas, Oklahoma, Iowa, Michigan, Nebraska, Idaho, Minnesota, New Hampshire, New Mexico, Kansas, North Dakota, Washington, Alaska, Oregon, Montana, South Dakota, Wisconsin, California, Colorado and Kentucky.
CMS Rule Permitting Such Opt-Outs (21 states and Guam as of 2020)
- Iowa opted out of the federal supervision requirement in December 2001.
- Nebraska opted out in February 2002.
- Idaho opted out in March 2002.
- Minnesota opted out in April 2002.
- New Hampshire opted out in June 2002.
- New Mexico opted out in November 2002.
- Kansas opted out in March 2003.
- North Dakota opted out in October 2003.
- Washington opted out in October 2003.
- Alaska opted out in October 2003.
- Oregon opted out in December 2003.
- Montana opted out in January 2004 (Gov. Judy Martz opted-out; Gov. Brian Schweitzer reversed the opt- out in May 2005, without citing any evidence to justify the decision. Subsequently, after the governor and his staff became more familiar with the reasons justifying the January 2004 opt-out, Gov. Schweitzer restored the opt-out, therefore, is currently in effect.)
- South Dakota opted out in March 2005.
- Wisconsin opted out in June 2005.
- California opted out in July 2009.
- Colorado opted out in September 2010 (for Critical Access Hospitals (CAHs) and specified rural hospitals)
- Kentucky opted out in April 2012.
- Guam opted out in June 2016.
- Arizona opted out in March 2020.
- Oklahoma opted out in August 2020.
- Michigan opted out in May 2022
- Arkansas opted out in May 2022
CRNAs: The Future of Anesthesia Care Today

